Introduction
The human heart, with its rhythmic and steady beats, has always held a certain mystery. For centuries, deciphering its patterns and understanding its anomalies remained a challenge. Enter the ECG machine—a revolutionary invention that demystified the heart's electrical symphony. In the annals of medical history, few devices can claim the transformative power that the Electrocardiogram (ECG) machine possesses. Since its inception, the ECG has not only granted us an intimate glimpse into the heart's inner workings but has also radically reshaped the landscape of cardiology. With the ability to detect irregularities, predict potential issues, and guide treatment options, the ECG machine has firmly cemented its place as an indispensable tool in cardiac care. This narrative aims to trace the journey of this remarkable device, from its embryonic beginnings to its current-day sophistication, illuminating its undeniable significance in the realm of medicine.

The Pioneers
The realm of cardiology, especially in its nascent stages, was akin to an uncharted map—a vast territory brimming with mysteries waiting to be unveiled. Within this expanse, the early 19th and 20th centuries witnessed groundbreaking discoveries, primarily fueled by trailblazing individuals determined to uncover the heart's electric nuances. Augustus Waller, a British physiologist with an insatiable curiosity, was among the earliest to leave an indelible mark. In 1887, amidst the hallowed halls of St. Mary's Medical School in London, Waller astounded the scientific community by recording the first human electrocardiogram using a capillary electrometer. This groundbreaking endeavor, although in its infancy, hinted at the vast potential of tracking the heart's electric symphony.
However, while Waller set the ball rolling, it was a Dutch physician named Willem Einthoven who would truly revolutionize the field. Drawing inspiration from Waller's initial forays, Einthoven embarked on a journey of relentless refinement. By 1903, he had introduced the world to the string galvanometer, a remarkable invention that elevated the precision and fidelity of cardiac electrical recordings to hitherto unseen levels. Einthoven's brilliance wasn't limited to instrument design; he also conceived a standardized lead system, offering a structured lens through which the heart's signals could be systematically interpreted. This system became a cornerstone in the field, underpinning countless subsequent innovations.
Einthoven's relentless dedication and transformative innovations didn't go unnoticed. In recognition of his profound impact on medicine, he was honored with the Nobel Prize in Physiology or Medicine in 1924. This esteemed accolade was a testament to his pioneering spirit and the foundational role he played in shaping modern cardiology.
Together, through their seminal contributions, Waller and Einthoven ignited a torch that illuminated the path for countless researchers and practitioners. Their legacy, grounded in innovation and discovery, continues to reverberate through the corridors of cardiac science, reminding us of the indomitable spirit of human inquiry.
Einthoven's String Galvanometer
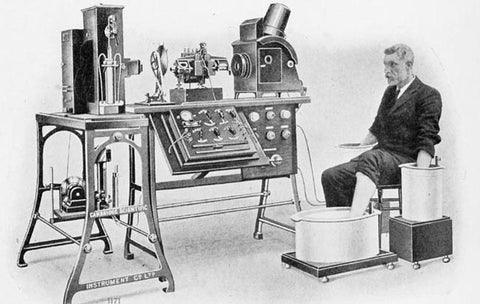
At the dawn of the 20th century, amidst a whirlwind of scientific and medical discoveries, emerged an invention that would transform the landscape of cardiology: Einthoven's string galvanometer. Conceived in 1903 by the Dutch physician Willem Einthoven, this device was a marvel of its time, combining meticulous engineering with a deep understanding of human physiology. Unlike its predecessors, which often provided imprecise and erratic recordings, the string galvanometer was revolutionary in its accuracy.
At its core, Einthoven's invention employed a fine quartz filament, or 'string', suspended between strong electromagnets. When exposed to the heart's electrical impulses, the string would move, and these movements were meticulously recorded on photographic plates. The resulting traces were unparalleled in their clarity and precision, revealing the heart's electrical activity with a detail never seen before. With this invention, the subtle nuances of the cardiac rhythm, from the smallest flutter to the pronounced spikes, could be captured and studied.
The string galvanometer not only provided an accurate representation of the heart's activity but also introduced a standardized method of recording. Einthoven meticulously categorized these recordings into what he termed as P, Q, R, S, and T waves—terminology that remains fundamental in ECG interpretation today. In essence, this invention was not merely a tool but a monumental leap in the realm of cardiac diagnostics. It shifted the understanding of the heart's electrical patterns from vague approximations to a concrete science.
While today's ECG machines have evolved with technological advances, the principles and foundations laid by Einthoven's string galvanometer remain deeply ingrained. This device, with its ingenious design and profound impact, stands as a testament to Einthoven's vision and the enduring legacy of early 20th-century medical innovation.
Evolution of Design and Usability
The journey of the ECG machine's design is a reflection of the broader narrative of medical advancement, mirroring our society's ever-evolving relationship with technology. In its infancy, the ECG apparatus was a colossal behemoth, occupying entire rooms, and demanding intricate setups. The early machines, like Einthoven's string galvanometer, while groundbreaking, were cumbersome and anchored to specialized locations. Their sheer size and complexity made spontaneous or frequent readings a challenging endeavor.
However, as the 20th century progressed, waves of technological innovations began to reshape the landscape. The miniaturization of electronics, bolstered by the semiconductor revolution, paved the way for more compact ECG designs. The once room-sized equipment began to condense into desk-sized, and eventually, handheld devices. This transformation wasn't just about size; it was about democratizing access. The advent of portable ECG machines meant that cardiac monitoring was no longer confined to specialized hospital rooms; it could now be conducted in clinics, ambulances, and even remote locations.
The latter half of the century and the onset of the 21st saw an increased focus on usability. Touchscreen interfaces, wireless capabilities, and intuitive software interfaces made the devices more user-friendly, reducing the learning curve and expanding their usage among varied healthcare professionals. The digital age further refined ECG technology, introducing features like automated interpretations, cloud storage of data, and seamless integration with other medical systems.
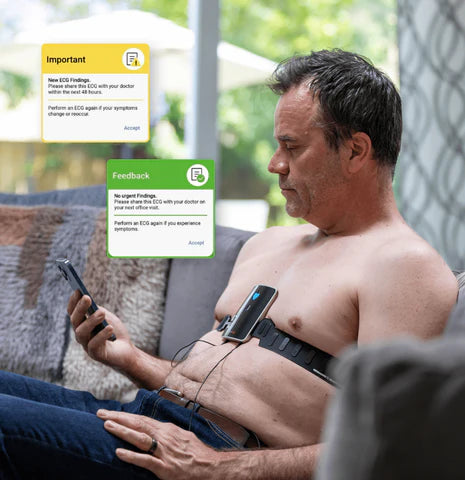
Moreover, the recent emergence of wearable technology and smartphone-compatible ECG monitors has revolutionized cardiac monitoring. Patients can now actively participate in their health management, monitoring their heart rhythms in real-time, and sharing data with healthcare providers instantaneously.
This evolutionary trajectory of the ECG machine, from gargantuan equipment to pocket-sized marvels, underscores the confluence of medical necessity and technological ingenuity. It's a testament to humanity's relentless pursuit of better, more accessible tools to safeguard our most vital organ.
The Introduction of the 12-lead Electrocardiogram
In the chronicle of cardiology's evolution, few innovations have had as profound an impact as the introduction of the 12-lead ECG. Prior to its inception, ECGs were limited in scope, capturing the heart's electrical activity from a handful of perspectives. While these early recordings were groundbreaking, they couldn't provide a comprehensive picture of the heart's multifaceted electrical symphony. Recognizing this limitation, pioneering cardiologists sought a more holistic approach to cardiac monitoring.
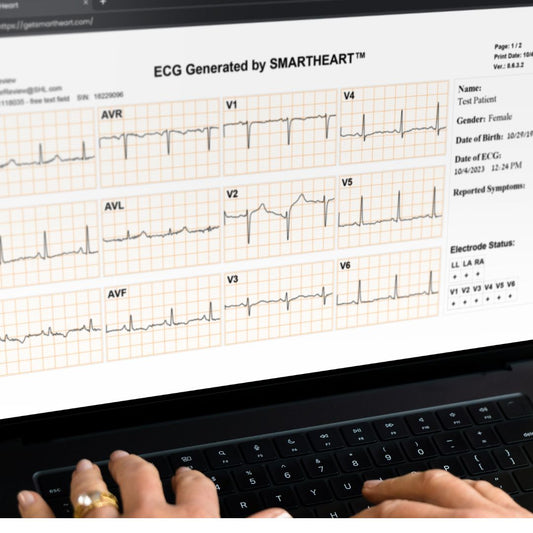
The 12-lead system emerged as a solution, offering a 360-degree view of the heart's electrical activity. By placing ten electrodes on the patient's body - four on the limbs and six on the chest - the system captures twelve distinct electrical viewpoints (or 'leads'). These twelve perspectives are invaluable, as they enable physicians to pinpoint specific areas of the heart where abnormalities may occur. Whether it's detecting a myocardial infarction's location, recognizing rhythm abnormalities, or identifying signs of electrolyte imbalances, the 12-lead system offers unparalleled diagnostic precision.
Beyond its technical prowess, the 12-lead test’s real triumph lies in its universality. Over time, it became the gold standard in ECG diagnostics worldwide. Its consistent methodology allows for reproducibility and comparability across different clinical settings and geographies. Whether in a state-of-the-art hospital in New York or a remote clinic in Nairobi, the 12-lead ECG provides the same reliable, comprehensive insights into the heart's wellbeing.
In essence, the adoption of the 12-lead ECG was more than just a technical upgrade; it was a paradigm shift. It underscored the medical community's commitment to standardized, comprehensive care, ensuring that no nuance of the heart's electrical dance went unnoticed. Through this journey, cardiology took a monumental step forward, fortifying its arsenal in the unending quest to understand and safeguard the human heart.
Digital Revolution
The digital age, marked by the confluence of computing power and innovative software, ushered in a transformative era for countless fields, with cardiology being no exception. As the world rapidly embraced the digital realm, so too did the domain of ECG technology, leading to enhancements that would revolutionize the very fabric of cardiac care.
Initially, ECG recordings were analog, with traces physically printed on paper. While this method provided valuable insights, it had its limitations. Storing vast amounts of paper recordings was cumbersome, and searching through archives was time-consuming. Enter the digital revolution. With the ability to convert cardiac electrical signals into digital data, storage became infinitely more efficient. Entire patient histories could be compressed and stored in compact digital spaces, accessible at the click of a button.
Beyond storage, the analytical capabilities brought forth by digital technology were game-changing. Advanced software could now instantly interpret ECG readings, identifying anomalies and patterns with remarkable accuracy. This not only expedited diagnosis but also minimized human error, providing healthcare professionals with a reliable second opinion. Moreover, digital platforms enabled seamless integration with other medical systems, allowing for a holistic view of patient health by collating data from various sources.
The interconnectedness of the digital age further elevated the ECG's potential. Cloud technology meant that ECG data could be shared instantaneously across the globe. A physician in Tokyo could review a patient's heart rhythms recorded in Paris just moments earlier, facilitating global collaboration and telemedicine.
Additionally, the integration of artificial intelligence and machine learning introduced a new frontier. These technologies began to assist in detecting complex patterns and predicting potential cardiac events, often before they became symptomatic.
In essence, the digital revolution didn't merely enhance the ECG; it redefined it. By intertwining the timeless principles of cardiology with the boundless possibilities of digital technology, the ECG transformed from a singular diagnostic tool to an interconnected beacon of modern medical marvel.
Modern Innovations
The trajectory of ECG technology is one marked by relentless innovation, with recent years witnessing leaps that once bordered on science fiction. As the line between healthcare and technology continues to blur, a new generation of ECG tools emerges, perfectly attuned to the demands and rhythms of contemporary life.
One of the most significant breakthroughs has been the rise of wearable ECG monitors. These compact devices, often integrated into smartwatches or fitness bands, allow for continuous heart monitoring. Whether it's an athlete tracking their heart rate during a strenuous workout or an individual with cardiac concerns keeping tabs on their rhythms, wearable ECGs provide real-time data, marrying convenience with cutting-edge technology. This continuous monitoring has proven invaluable in detecting arrhythmias that might be sporadic and missed during a traditional ECG session.
Complementing wearables are smartphone-based ECG apps, democratizing cardiac care like never before. With the ubiquity of smartphones, heart monitoring is no longer confined to medical settings. By using specially designed sensors that pair with dedicated apps, individuals can capture ECG readings from virtually anywhere, transmitting this data to healthcare professionals or storing it for future reference. Such innovations bring cardiac diagnostics to the palms of our hands, fostering a proactive approach to heart health.
Yet, perhaps the most groundbreaking advancement resides in the realm of artificial intelligence (AI). AI-enhanced interpretation tools are beginning to play pivotal roles in analyzing the vast amounts of data generated by ECGs. These algorithms, trained on millions of ECG tracings, are capable of identifying subtle patterns and abnormalities that might elude even the most trained human eye. By providing instantaneous, accurate interpretations, AI aids in rapid diagnostics, especially crucial in life-threatening situations.
In summary, the modern chapter in the ECG saga is one of empowerment and accessibility. With tools that integrate seamlessly into daily life and algorithms that push the boundaries of what's possible, ECG technology stands at the forefront of a new age in cardiac care, where prevention, early detection, and global collaboration are not just ideals, but realities.
Conclusion
From its humble beginnings in the hands of pioneers like Waller and Einthoven to the sophisticated marvels of the digital age, the ECG machine's odyssey is a testament to humanity's undying quest for knowledge and betterment. This once-massive apparatus, rooted in rooms of intricate machinery, has metamorphosed into sleek wearables and apps that sit comfortably on our wrists and phones. At its core, the ECG's evolution captures the essence of medical innovation: the marriage of curiosity with necessity, underpinned by technological prowess.
In contemporary medicine, the ECG stands not merely as a diagnostic tool but as a symbol of how far we've come. It remains a cornerstone, an unwavering sentinel in our relentless pursuit to understand and protect the heart—a testament to its enduring significance. Yet, as we stand on the cusp of a future brimming with potential, one can't help but wonder: what's next? With the rapid strides in AI, quantum computing, and bioengineering, the horizon promises innovations beyond our current imagination.
In reflecting upon the ECG's storied past, we are reminded of the boundless possibilities that await. The heart, with its rhythmic beats and electric dances, will continue to inspire, challenge, and drive us forward, and in this journey, the ECG machine—ever-evolving and indispensable—will undoubtedly remain our trusted companion.